Estrogen and Menopausal Psychosis: Exploring the Link
Find out how fluctuating estrogen and menopausal psychosis may be connected. Learn symptoms, causes, what's normal and what's not.
MENOPAUSAL MENTAL HEALTHMENOPAUSAL SYMPTOMS
Kennerly Clay
12/17/20245 min read


Are you experiencing mood swings that feel more intense than usual? Finding yourself questioning reality in ways you never have before? Many women find themselves grappling with unexpected mental health challenges in menopause, and you may be wondering whether these experiences could be signs of something more serious, like psychosis.
In this article, we'll explore the complex relationship between estrogen, menopause, and mental health, helping you understand what's normal, what's not, and when to seek help.
If you or someone you know is in crisis, please call 988, the Suicide & Crisis Lifeline in the United States.
Can too much estrogen cause psychosis?
Excessive estrogen levels are not typically associated with causing psychosis. In fact, research suggests that estrogen generally has a protective effect against psychotic symptoms. The "Estrogen Protective Hypothesis" posits that estrogen helps shield women from psychosis, with episodes of psychosis occurring more frequently during periods of low estrogen levels.
Facts on estrogen and psychosis
Low estrogen, not high estrogen, is linked to increased psychosis risk.
Psychotic episodes are more common during estrogen withdrawal periods, such as:
First stage of menses
After discontinuing oral contraceptives or estrogen replacement
Post-abortion
Postpartum
After menopause
Estrogen enhances dopamine receptor sensitivity, potentially making antipsychotics more effective.
The neuroprotective effects of estrogen are widely accepted, explaining the later onset of psychosis in women compared to men.
Estrogen deficiency, rather than excess, is common in both women and men with schizophrenia.
While estrogen plays a complex role in mental health, current evidence does not support the notion that too much estrogen causes psychosis. Instead, it suggests that maintaining adequate estrogen levels may help protect against psychotic symptoms in vulnerable people.
Menopause survival tip sheet
The Menopause Madness Relief Kit is a hand-curated list of menopausal survival tips from women who've been to hell and back.


Low estrogen, not high estrogen, is linked to increased psychosis risk.
Can menopause induce psychosis?
Menopause-associated psychosis (MAP) is a rare but recognized phenomenon. The menopausal transition can be a vulnerable period for some women, potentially triggering new-onset psychosis or exacerbating existing conditions. This "second period of risk" for psychosis, after adolescence and early adulthood, is thought to be linked to the significant hormonal changes occurring during this time.
What are the symptoms of hormonal psychosis?
Menopause psychosis symptoms can include delusions, hallucinations, and a break from reality. These symptoms may be accompanied by other menopausal experiences such as mood swings, anxiety, and cognitive changes. It's important to note that while these symptoms can be distressing, they are manageable with proper treatment.
MAP can present with a range of symptoms that may be distressing for women experiencing them. Some examples of symptoms associated with MAP include:
Positive psychotic symptoms
Delusions - False beliefs that persist despite evidence to the contrary
Hallucinations - Perceiving things that aren't actually present
Cognitive symptoms
Difficulty concentrating
Impaired short-term memory
Mood disturbances
Anxiety
Irritability
Depressive symptoms
Sleep disturbances
Exacerbation of pre-existing mental health conditions, such as schizophrenia or bipolar disorder
And here are some real-life examples of what a woman might experience with MAP:
A woman in her late 40s suddenly starts hearing voices criticizing her actions, despite never having experienced hallucinations before.
A 52-year-old woman develops an unshakeable belief that her neighbors are spying on her, even though there's no evidence to support this idea.
A previously high-functioning executive in her early 50s finds herself struggling to remember important details at work and has difficulty focusing during meetings.
A woman approaching menopause experiences severe mood swings, crying uncontrollably one moment and feeling inexplicably angry the next.
A 55-year-old woman with a history of well-managed schizophrenia notices a sudden increase in the frequency and intensity of her psychotic symptoms as she enters menopause.
It's important to note that while these symptoms can be alarming, they are treatable. And more importantly, some of these experiences may not be signs of menopausal psychosis. If you’re experiencing such symptoms, be sure to consult with a healthcare provider for proper evaluation and management.
Some of these experiences may not be signs of menopausal psychosis.
What causes psychosis to flare up?
Contrary to what you might expect, it's not high estrogen psychosis we're concerned about, but rather the sudden decline in estrogen levels that may trigger psychotic symptoms. As previously mentioned, the "Estrogen Protective Hypothesis" suggests that estrogen acts as a shield against psychosis, and its rapid decrease during menopause may leave some women vulnerable.
Can menopause cause bipolar disorder?
While menopause doesn't directly cause bipolar disorder, it can significantly impact existing conditions. Menopause bipolar disorder symptoms may worsen during this transition. Women with bipolar disorder often experience more severe depressive episodes and mood elevation during the late menopausal transition and early postmenopause.
If you're experiencing any concerning symptoms, be sure reach out to a trusted healthcare provider. Don't wait for symptoms to get worse!
The information provided in this blog post is for educational purposes only and should not be considered medical advice. Every individual's situation is unique, and what works for one person may not be suitable for another. Always consult with a qualified healthcare provider before making any changes to your treatment plan or starting new medications. Your healthcare provider can take into account your personal medical history, current health status, and other individual factors to determine the most appropriate course of action for your specific needs.
Wanna connect further on estrogen and psychosis in menopause?
About the author
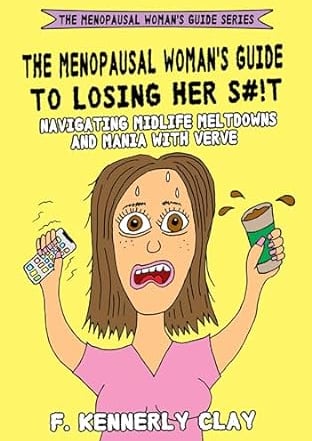
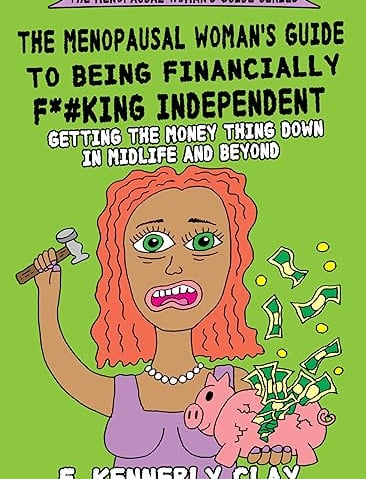
Kennerly Clay is the author of The Menopausal Woman's Guide series, a snarky trilogy for women who are losing their shit in peri/menopause. Her focus is on all things mental health, financial health, and personal growth during the menopausal years.
Books for women who are losing it in menopause
Mental Health
Losing your mind in peri/menopause?
The menopausal woman's guide series
Financial Health
Had enough of financial insanity?
Personal Growth
Triggers? Old stuff kicking up?
Related topics
Explore helpful articles, tips, and advice for women who are losing their shit in menopause.
Community
Stay Connected
© 2024. Eclectic Content, Inc. All rights reserved.